OVERVIEW
One of the most feared words that any patient can hear is C-A-N-C-E-R!
Despite the fact that billions of rands are spent annually on cancer research world-wide, we as oculatrists regularly see patients in our rooms that are either recovering from some form of cancer or has had previous treatment for cancer.
Cancer is caused by healthy cells growing uncontrollably and then forming a mass called a tumor. Early detection is the key to successful treatment and in most cases survival. Information regarding symptoms and signs can empower the ocularist to advise and refer patients for early detection. Skin defects and tumors in and around the eyelids should be a red light to any ocularist and a discussion with the patient regarding a referral is very important. According to a study at the Johns Hopkins School of Medicine, Baltimore, the most common symptoms for skin cancer on the eyelids are tumors, ulcerations or sores, red spots and trichiasis or ingrown eyelashes., all symptoms and indications (signs) that can be an early warning to the ocularist for referral.
CANCER IN AND AROUND THE EYELIDS
Eyelids are a highly specialized region of the ocular adnexa. It consists of multiple tissue types which have the potential to give rise to benign and malignant lesions. Tumors inside or outside the eyelids can be cancerous or benign. Cancerous tumors are malignant. This causes them to grow and spread to other parts of the body. The ocularist should be aware of any changes, swelling or other abnormalities regarding the eyelids. It is in the interest of the patient to make them aware of these abnormalities that may, in some cases, be an early indication of cancer.
In countries where exposure to the sun is high, such as South Africa, skin cancer is very common. Eyelids are one of the most common places where skin cancer occurs. Basal cell cancer is the most common eyelid cancer found, almost 90%.
Eyelid cancer can be identified by the following signs:
- Change in appearance of the skin of the eyelid
- Swelling of the eyelid
- Thickening of the eyelid
- Eyelid having chronic infection
- An ulceration (area where skin is broken) on the eyelid that does not heal
- A spreading, coloured mass on the eyelid
- Flaking or scaling of the eyelids
Any of these symptoms or signs detected should be referred by the ocularist to a specialist for diagnosis and treatment.
EPITHELIAL TUMORS
Cancer of the eyelid, inside or outside on the outer surface, is categorized as an epithelial tumor. Eyelid tumors can originate from fat (sebaceous), sweat or apocrine glands. There are a few common types of cancers occurring in and on the eyelids.
Basal cell carcinoma
Basal cells are found under the squamous cells in the lower epidermis. Basal cells are round in shape. Sun exposure is the biggest cause of cancer of these cells. Nearly 80% of skin cancers occur in this layer of the skin. Fair skinned people with light eyes are more prone to this cancer. It normally appears in the lower lid of the eye.
Signs and symptoms of basal cell carcinoma
The following are signs and symptoms of basal cell carcinoma:
- A reddish nodule slowly forming on the eyelid
- Tumor that is most commonly found on the lower eyelid followed by the medial canthus (toward the nose)
- Eyelash loss (around the tumor) suggests that a tumor is malignant.
- Tumor growing within the eyelid (not making a nodule), can cause “pulling” of the eyelid (away from the prosthesis)
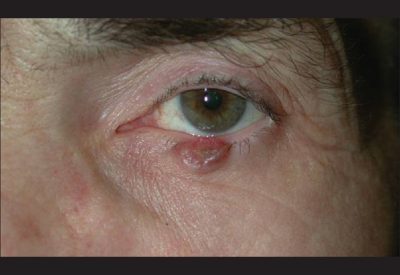
Sebaceous carcinoma
Sebaceous carcinoma may start from meibomian glands (glands that discharge a fatty secretion) and occur mostly in middle age and older adults. It is an aggressive cancer that normally occurs on the upper eyelid and is associated with radiation exposure. It can also start at the glands of Zeis (sebaceous glands) found at the base of the eyelashes.
Signs & symptoms of sebaceous carcinoma
The following are signs and symptoms of sebaceous carcinoma:
- A solitary eyelid nodule (eyelid “hanging” or pushing over the prosthesis)
- Diffuse eyelid thickening, sometimes with loss of cilia.
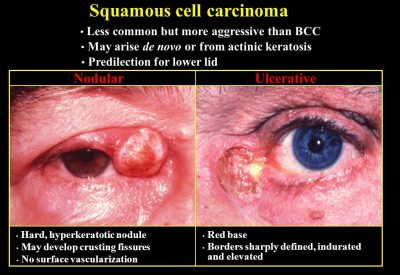
Squamous cell carcinoma
The top layer of the epidermis is mostly made up of squamous cells. As this is the layer of the skin mostly exposed to the sun, it is no wonder that up to 30% of skin cancers begin in this layer. Other causes of cancer in this layer may be exposure to x-rays, burned skin and chemically damaged skin. Although basal cell carcinoma is more common, squamous cell carcinoma is much more aggressive and can spread to nearby tissue.
Signs & symptoms of squamous cell carcinoma
The following are signs and symptoms of squamous cell carcinoma
- Red inflamed lesion with white flaky surface
- Thickened well-demarcated reddish, flat tumor surrounded by inflammation
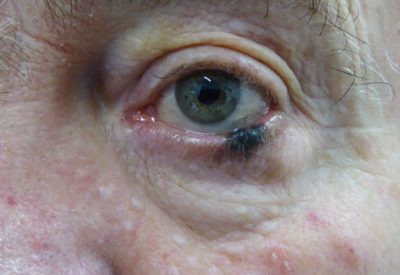
Melanoma
Melanocytes are scattered cells found in the deepest layer of the epidermins. Melanocytes produce melanin that gives color to the skin. Melanoma starts in these cells and is the most dangerous of all skin cancers. Fortunately melanoma of the eyelids is very rare.
“Early-stage ocular melanoma may display mild or no symptoms, and doctors sometimes detect it during routine eye exams” according to Medical News Today. This is why it is so important for the ocularist to inform the patient of any discolouring, spots or pigmentation of the eyelids.
Signs & symptoms of melanoma
The following are signs and symptoms of melanoma:
- Discolouring of the eyelids
- New spots and pigmentation of the eyelids
In general, basal cell and squamous cell skin cancer is almost always curable, especially if the cancer is found and treated early. Melanoma is also highly curable if it is diagnosed and treated in its earliest stages. However, melanoma is more likely to spread to other parts of the body. Therefore it is recommended that the ocularist takes a close-up photo of the patients’ eyes and eyelids for reference, if any differences in appearance occur on the annual polish, build-ups, etc.
TREATMENT OF EYELID CANCER
It is unfortunate that some of the patients seen and referred by the ocularist will indeed be diagnosed with some form of eyelid cancer. A diagnosis can be made by a biopsy or various other tests. Imaging tests can show whether the cancer has spread. The following factors are considered when specialists perform diagnostic tests:
- Age of the patients
- Current medical condition of patient
- Medical history of patient
- Signs and symptoms
- Type of cancer suspected
STAGES OF EYELID CANCER & TREATMENT
Once the stage of the eyelid cancer has been determined a prognosis can be made and the best kind of treatment can be started. It often requires a multidisciplinary team (different types of doctors and other role-players) to work together to create an overall treatment plan for the patient. For eyelid cancer, this team may include dermatologists, surgeons, radiation oncologists, ophthalmologists, general practitioners, etc. Treatment may include surgery, radiotherapy, chemotherapy, hormone therapy, active surveillance and palliative care.
The ocularist will also play an important role in the holistic approach to the overall well-being of the patient. When fitting the prosthesis the ocularist must be aware of current eyelid cancer treatment. Continued treatment may influence the socket and the eyelids in terms of the flexibility of the skin and even the shape and size. In such cases it may be necessary to postpone the fitting of the prosthesis for the optimal benefit of the patient.
SURGERY
For this article we are only going to look at surgery options.
Surgery of the eyelid
In the event of surgery required to remove the tumor, some healthy tissue from the lid will also have to be removed from both sides of the tumor. Where the tumor is very large, it may require extensive surgery and cause scarring and deformity of the eyelid.
Whether the eyelid is that of an empty socket or the normal eye, it will have an influence on the shape of the eyelids. This can cause many headaches for the ocularist striving to maintain similarity in shape and size of both sockets. Surgery can also involve enucleation (removal of the eye) where the tumor is inside the eye or eyelid.
After surgery or radiation therapy, the eyelids can roll inward (entropion) or sag outwards (ectroption). This can cause problems when fitting an ocular prosthesis or even eye health problems with the normal eye. Fortunately it can be repaired surgically. The ocularist should be aware of this and discuss the possibilities of referral to a plastic surgeon or ophthalmologist with the patient.
Biopsy
A part of the tumor or even the whole tumor may be removed by surgical biopsy. In the case of a cancerous tumour, an excisional biopsy may be the only treatment needed, if enough healthy tissue has been removed with the surgical biopsy.
Mohs’ surgery
Removal of small fragments of the edge of where the tumor is situated is called Mohs’ surgery. This is used for tumors in hard-to-reach places, very large tumors and where tumors have reoccurred (re-grown) in the same place. In some cases patients will need reconstructive surgery after Mohs’ surgery.
Cryosurgery
Cryosurgery uses liquid nitrogen to freeze and kill cells. Blisters will later form on the lid and shed off.
Reconstructive surgery
There are many cases where patients will need reconstructive surgery after eyelid cancer was diagnosed and treated. Skin grafts may be used to completely reconstruct the eyelid to obtain a “normal” appearance. In the case of an empty socket, where surgery was also required on the lid, be it bottom- or top lid, it may have a direct influence on the making and fitting of an ocular prosthesis and obtaining similarity. The ocularist will sometimes need to add on a prostheses or trim and re-shape after surgery to obtain the required size and form.
CONCLUSION
In conclusion we can see that it is very important to do a thorough check-up of the socket and the eyelids on the annual polish consultation of every patient. Any abnormalities, swelling, thickening of the eyelids, red or dark marks, flaky or scaly appearance should be considered for referral and should be discussed with the patient. Unfortunately cancer of the eyelids can reoccur. Early detection and referral for diagnosis by a specialist is part of the overall holistic care given to our patients.
REFERENCES
- http://www.asoprs.org/i4a/pages/index.cfm?pageid=3679
- http://www.cancer.net/cancer-types/eyelid-cancer
- http://www.cancer.org/cancer/eyecancer/detailedguide/eye-cancer-what-is-eye-cancer
- http://www.oculist.net/downaton502/prof/ebook/duanes/pages/v4/v4c003.html
- http://www.ijo.in/article.asp?issn=0301-4738;year=2016;volume=64;issue=3;spage=177;epage=190;aulast=Pe%92er
- https://eyecancer.com/eye-cancer/conditions/eyelid-tumors/squamous-carcinoma-eyelid/
- https://www.aao.org/eyenet/article/diagnosis-management-of-sebaceous-carcinoma-of-eye
- https://www.reference.com/health/melanoma-eyelid-c27a1b9070c7934e?qo=cdpArticles
- http://www.skincancer.org/prevention/sun-protection/for-your-eyes/the-eyelids-highly-susceptible-to-skin-cancer
- Google Images